Recovering from bariatric surgery is not only about diet, weight loss, or wound healing. A critical but often overlooked part of recovery is respiratory rehabilitation. Breathing exercises play a structured role in early healing, pain management, mobility, and long-term lung health.
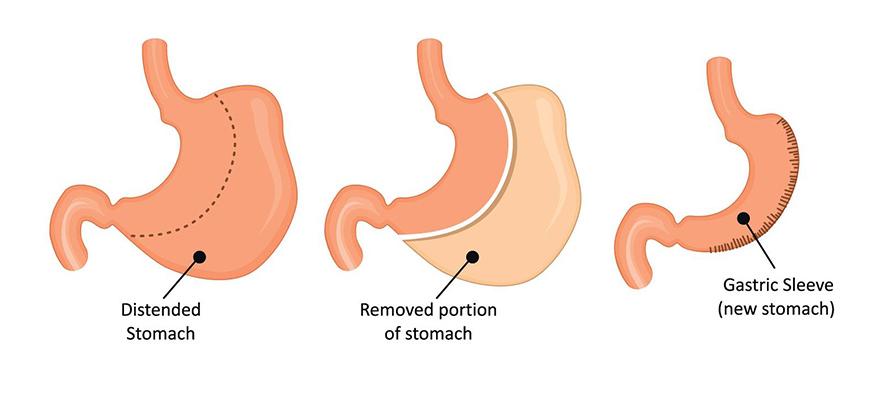
In modern bariatric programs, especially in gastric sleeve surgery, respiratory training begins immediately after surgery and continues throughout the first weeks of recovery.
These exercises are not random practices; they are medically guided techniques designed to prevent complications, support circulation, and help patients regain normal breathing patterns after anesthesia and abdominal surgery.
Many patients assume that breathing will naturally return to normal after surgery. However, abdominal procedures temporarily alter posture, muscle function, and lung expansion.
Without proper guidance, shallow breathing can increase the risk of lung congestion, infection, or delayed recovery. For this reason, structured breathing exercises are integrated into post-operative care plans across major bariatric centers.
Why Breathing Exercises are Helpful After Bariatric Surgery?
Any abdominal surgery affects how a person breathes. The diaphragm, which is the main muscle of respiration, works closely with the abdominal wall. After gastric sleeve surgery, temporary swelling, pain, and muscle guarding can limit deep breathing.
Patients often instinctively take short, shallow breaths to avoid discomfort, but this pattern reduces lung ventilation and increases the risk of complications. Proper breathing exercises help re-expand the lungs, improve oxygen delivery to healing tissues, and minimize post-operative fatigue.
They also support blood circulation, which is essential for wound repair and preventing blood clots. Doctors emphasize that respiratory training is as important as walking and nutrition in the early recovery phase.
How Surgery Affects Lung Mechanics?
During anesthesia, normal breathing patterns are temporarily suppressed, and the lungs may not fully expand. In addition, the surgical position and abdominal incisions can slightly restrict chest movement. These factors can cause small areas of the lung to collapse, a condition known as atelectasis.
Breathing exercises counteract this by encouraging full lung inflation and gradual muscle relaxation. Patients who consistently practice deep breathing typically experience less chest tightness, fewer respiratory symptoms, and a smoother overall recovery.
Early Post-Operative Breathing Protocol in Hospitals
In the first hours after gastric sleeve surgery, nurses and physiotherapists introduce gentle breathing techniques while patients are still in bed. The goal is to restore normal lung function as early as possible. Patients are taught to take slow, controlled breaths rather than rapid or forceful inhalations.
Most hospitals encourage patients to sit upright as soon as they are medically stable. This position naturally improves lung expansion and makes breathing exercises more effective. Medical teams monitor oxygen levels, breathing patterns, and overall comfort to adjust techniques accordingly.
Diaphragmatic Breathing Step-by-Step
One of the foundational techniques taught after the gastric sleeve in Istanbul is diaphragmatic breathing, also called belly breathing. Patients place one hand on their chest and the other on their abdomen.
They are instructed to inhale slowly through the nose, allowing the abdomen to rise while keeping the chest relatively still. On exhalation, patients gently release the air through pursed lips, feeling the abdomen fall.
This pattern strengthens the diaphragm, reduces tension, and promotes deeper lung ventilation. Surgeons and physiotherapists often recommend repeating this exercise several times per hour in the first few days after surgery.
Incentive Spirometry and Mobility
Many bariatric centers provide an incentive spirometer, a small device that visually guides patients to take slow, deep breaths. Patients are encouraged to use it regularly, usually every one to two hours while awake. The device helps ensure that breathing is deep enough to expand the lungs fully.
Clinics offering gastric sleeve surgery in Turkey often combine spirometry with light movement. Even short walks around the hospital corridor support lung clearance and reduce the risk of fluid buildup in the lungs. Movement and breathing work together to accelerate recovery.
Coordinating Breathing with Walking
Walking after surgery is essential, but how a patient breathes while walking matters just as much. Patients are taught to synchronize their steps with slow inhalations and exhalations. This rhythmic pattern prevents breathlessness and improves stamina.
Rather than rushing, patients are encouraged to walk at a steady pace, breathing deeply and evenly. Over time, this coordination becomes natural and supports both respiratory and cardiovascular recovery.
Pain Control, Posture, and Breathing
Post-operative discomfort can discourage deep breathing. However, avoiding deep breaths can slow recovery. Doctors advise patients to take pain medication as prescribed so they can perform breathing exercises comfortably. Proper pain management enables fuller lung expansion and reduces tension in the chest and abdomen.
Good posture is equally important. Slouching compresses the lungs and makes breathing shallow. Patients are taught to sit and stand tall, allowing the rib cage to expand freely with each breath.
Positioning Strategies to Improve Lung Expansion
Lying flat immediately after surgery can limit breathing depth. Many patients are advised to sleep with their upper body slightly elevated. This position reduces pressure on the diaphragm and makes breathing easier.
Side-lying positions may also be recommended once patients are stable, as they can help redistribute lung ventilation and improve oxygenation. These adjustments are usually guided by medical staff based on individual needs.
Preventing Complications Through Respiratory Training
Consistent breathing exercises significantly lower the risk of pneumonia, atelectasis, and prolonged oxygen dependency. Patients who actively engage in respiratory rehabilitation tend to recover faster and experience fewer post-operative respiratory issues.
In gastric sleeve turkey programs, respiratory care is considered a preventive measure rather than a reaction to complications. The emphasis is on maintaining lung health from day one of recovery.
Warning Signs that Require Medical Review
While breathing exercises are generally safe, patients should be aware of symptoms that need medical attention. These include persistent shortness of breath, chest pain, fever, severe coughing, or bluish discoloration of lips or fingertips.
Doctors instruct patients to report these symptoms immediately rather than attempting to manage them alone. Early intervention is key to preventing serious complications.
At-home Breathing Plan During Recovery
Once discharged, patients continue their breathing exercises at home. During the first week, deep breathing is usually performed several times per day, gradually becoming less frequent as lung function normalizes.
Light walking, gentle stretching, and upright posture remain important. Patients are advised to avoid strenuous activity until cleared by their medical team, but regular movement supports respiratory health.
Progression Over the First Four Weeks
In the second week, many patients feel more comfortable breathing deeply without conscious effort. Exercises shift from structured drills to more natural breathing during daily activities.
By weeks three and four, patients often incorporate breathing techniques into light exercise routines such as slow walking or stretching. This gradual progression helps rebuild endurance safely.
Role of the Multidisciplinary Team
Respiratory recovery is not managed in isolation. Surgeons, nurses, physiotherapists, and dietitians collaborate to support each patient’s healing. Regular follow-ups allow doctors to assess lung function, mobility, and overall recovery.
Before and after gastric sleeve surgery, patients receive clear doctor’s advice regarding breathing techniques, activity levels, and warning signs. These recommendations are tailored to individual medical histories rather than applied as generic rules.
Leading bariatric centers in gastric sleeve, Istanbul, education is a central part of care. Patients are not just told what to do; they are taught why each exercise matters. This understanding improves compliance and long-term success.
Frequently Asked Questions
Why are breathing exercises necessary after gastric sleeve surgery?
Breathing exercises help re-expand the lungs after anesthesia, reduce the risk of lung complications, improve oxygen delivery to healing tissues, and support overall recovery by preventing shallow breathing patterns.
How soon should I start breathing exercises after surgery?
Most patients begin gentle breathing techniques within hours of waking from anesthesia under nurse or physiotherapist supervision, as long as they are medically stable.
How often should I practice breathing exercises at home?
During the first week, many doctors recommend performing deep breathing exercises several times daily, gradually reducing frequency as normal breathing returns.
Can breathing exercises reduce post-operative pain?
While they do not eliminate pain, controlled breathing can reduce muscle tension, improve relaxation, and make movement more comfortable when combined with prescribed pain management.
When should I contact a doctor about breathing problems?
You should seek medical advice if you experience persistent shortness of breath, chest pain, fever, severe coughing, or difficulty breathing despite regular exercise.